The occipital lobe is the brain’s visual processing center. Located at the back of the head, it helps us make sense of what we see—from colors and shapes to motion and depth.
Though it’s the smallest of the four major brain lobes, it’s crucial for everyday activities like reading, recognizing faces, and navigating the world.

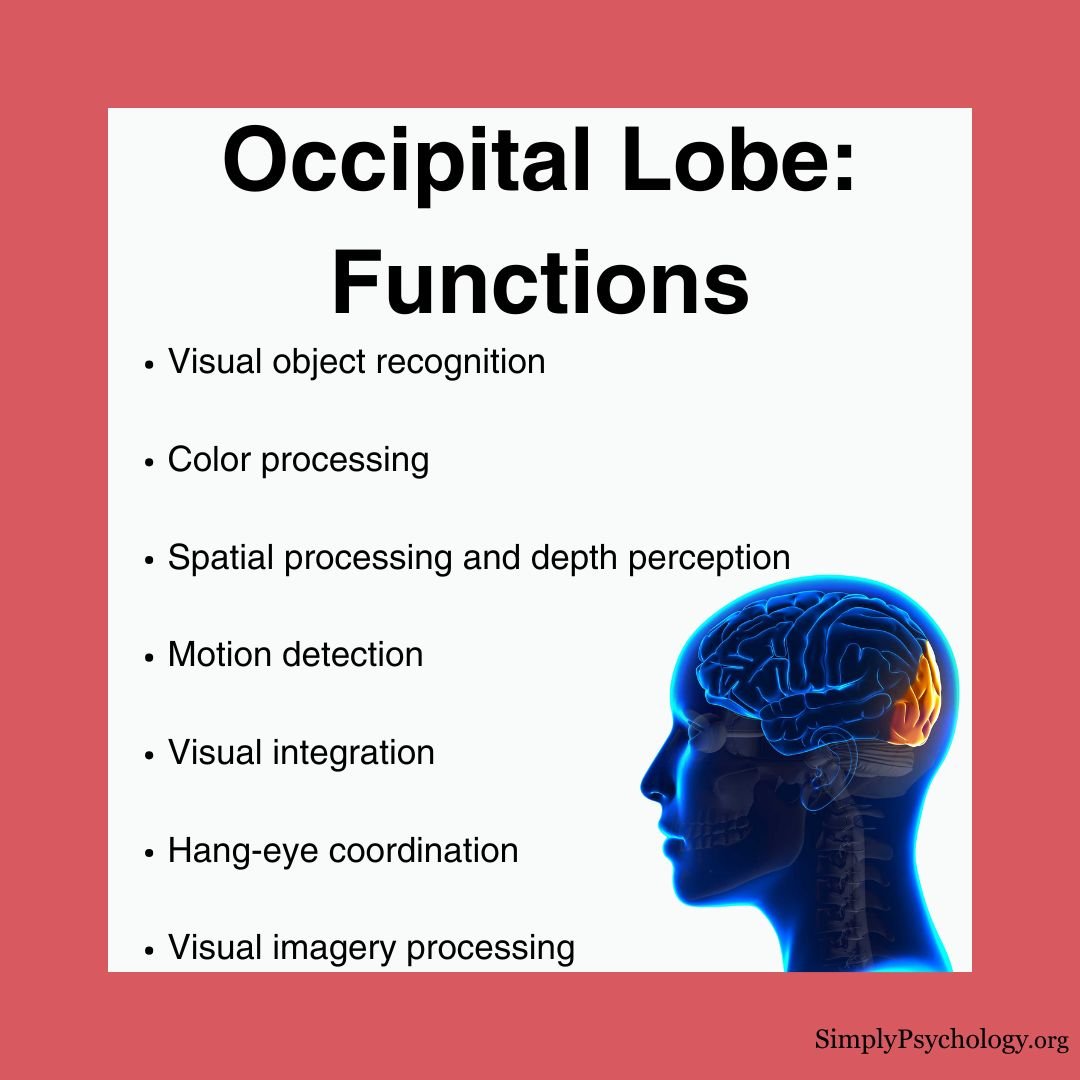
Key Functions of the Occipital Lobe
The occipital lobe handles a wide range of visual processing tasks. Here’s what it does:
1. Visual Recognition
- Identifies faces, objects, and written words
- Distinguishes fine details like texture, shape, and pattern
- Helps mentally rotate or imagine objects from different angles
2. Spatial and Motion Processing
- Maps the 3D world and calculates distance
- Supports depth perception and hand-eye coordination
- Tracks the movement and direction of objects
3. Color Perception
- Translates light wavelengths into color
- Helps us recognize color in different lighting
- Detects subtle color differences for tasks like matching shades
4. Integration With Other Brain Regions
- Works with the temporal lobe to identify and remember what we see
- Connects with motor areas to guide eye movements
- Coordinates with the parietal lobe for spatial awareness and mental imagery
Visual Phenomena Involving the Occipital Lobe
This lobe plays a surprising role in unique visual experiences:
- Dream imagery: It helps generate images we “see” in dreams.
- Synaesthesia: Some people experience colors when reading letters or numbers.
- Blindsight: People with damage to the occipital lobe may respond to visual cues without conscious awareness.
- Visual hallucinations: Damage or stimulation can produce vivid visual experiences.
Location
The occipital lobe is located at the very back of the brain beneath the occipital bone and behind the parietal and temporal lobes.
It is the smallest lobe of the brain, accounting for around 12% of the total surface area of the brain’s cortex.
There are two sides to the occipital lobes, in both the left and right hemispheres of the brain, separated by a cerebral fissure (a deep groove separating the two cerebral hemispheres).

Structure
The occipital lobes can be divided into several functional areas, although no anatomical markers distinguish these areas.
Brain imaging has revealed that neurons in the occipital cortex create an ongoing visual map of information taken in by the retinas.
Similarly, it is worth noting that the motor cortex plays a role in the muscles of the eyes, which are heavily relied on by the occipital lobes.
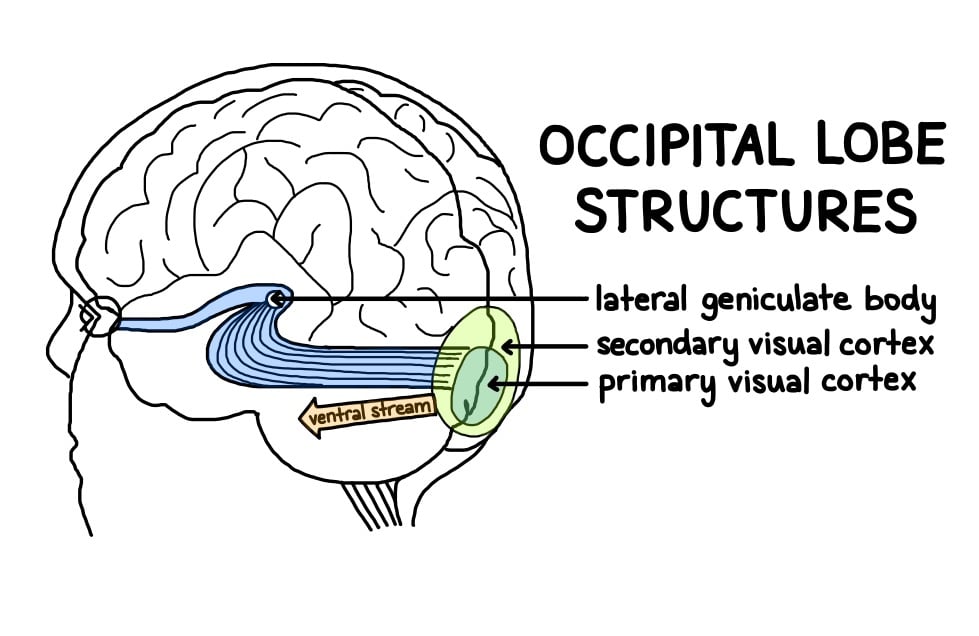
Primary Visual Cortex (V1 or Brodmann Area 17)
- Detects motion, light, color, and location
- First stop for visual information from the eyes
Secondary Visual Cortex (V2, Areas 18 & 19)
- Refines input from V1
- Passes information along to areas V3, V4, and V5 for further processing
Ventral Stream (“What” Pathway)
- Sends information to the temporal lobe
- Helps us understand what we’re seeing (e.g., recognizing a face or a cup)
Dorsal Stream (“Where” Pathway)
- Sends information to the parietal lobe
- Tells us where things are in space and how they’re moving
Lateral Geniculate Body and Lingula
- Help add depth and spatial clarity to what we see
- Relay stations that refine visual data before it reaches the cortex
What Happens When the Occipital Lobe Is Damaged?
Damage to the occipital lobe can affect visual perception in several ways:
Common Symptoms
- Partial or complete blindness
- Visual hallucinations
- Difficulty reading, writing, or recognizing objects
- Poor depth perception or motion tracking
- Inability to distinguish colors or shapes
How Damage Occurs
Injuries can result from trauma, stroke, tumors, or infections. Even small areas of damage can create “blind spots” in a person’s field of view.
In some cases, the brain adapts by rerouting information, but widespread damage may cause permanent vision loss.
Associated Conditions
Riddoch Syndrome
A rare condition associated with the occipital lobes is called Riddoch Syndrome. This is a condition whereby an individual is unable to view stationary objects in their field of vision. They can only, however, view people or objects if they are moving.
Autism
Studies using MRI have revealed significant occipital cortex enlargement in autistic individuals compared to control groups.
This structural difference correlates with enhanced perceptual abilities, particularly in visual search and discrimination tasks, where individuals with autism often outperform neurotypical participants.
Depression
Research using PET scans has identified a correlation between depression and reduced blood flow in the occipital lobe.
They found that successful pharmacotherapy treatment for depression can increase blood flow to the parieto-occipital regions, suggesting a previously unknown link between visual processing and mood disorders.
Epilepsy
Occipital lobe epilepsy presents unique challenges for treatment. While surgery can be successful, precise identification of the affected area through brain imaging remains difficult.
Studies have shown that individuals with occipital lobe epilepsy often demonstrate reduced performance in attention, memory, and intellectual functioning compared to control groups.
Schizophrenia
Brain imaging studies have revealed reduced gray matter volume in the visual association cortex of individuals with chronic schizophrenia.
This structural difference may explain some of the visual processing deficits commonly observed in schizophrenia patients.
The connection between occipital lobe abnormalities and visual hallucinations in schizophrenia continues to be an active area of research.
Binder, D. K., Von Lehe, M., Kral, T., Bien, C. G., Urbach, H., Schramm, J., & Clusmann, H. (2008). Surgical treatment of occipital lobe epilepsy. Journal of Neurosurgery, 109 (1), 57-69.
Gülgönen, S., Demirbilek, V., Korkmaz, B., Dervent, A., & Townes, B. D. (2000). Neuropsychological functions in idiopathic occipital lobe epilepsy. Epilepsia, 41 (4), 405-411.
Harward, S. C., Chen, W. C., Rolston, J. D., Haglund, M. M., & Englot, D. J. (2018). Seizure outcomes in occipital lobe and posterior quadrant epilepsy surgery: a systematic review and meta-analysis. Neurosurgery, 82 (3), 350-358.
Ishizaki, J., Yamamoto, H., Takahashi, T., Takeda, M., Yano, M., & Mimura, M. (2008). Changes in regional cerebral blood flow following antidepressant treatment in late‐life depression. International Journal of Geriatric Psychiatry, 23 (8), 805-811.
Jessell, T. M. (1991). Principles of neural science (pp. 173-193). J. H. Schwartz, & E. R. Kandel (Eds.). New York: Elsevier.
McCarley, R. W., Wible, C. G., Frumin, M., Hirayasu, Y., Levitt, J. J., Fischer, I. A., & Shenton, M. E. (1999). MRI anatomy of schizophrenia. Biological Psychiatry, 45 (9), 1099-1119.
Onitsuka, T., McCarley, R. W., Kuroki, N., Dickey, C. C., Kubicki, M., Demeo, S. S., Frumin, M., Kikinis, R., Jolesz, F. A. & Shenton, M. E. (2007). Occipital lobe gray matter volume in male patients with chronic schizophrenia: A quantitative MRI study. Schizophrenia Research, 92 (1-3), 197-206.
Park, K. C., Yoon, S. S., & Rhee, H. Y. (2011). Executive dysfunction associated with stroke in the posterior cerebral artery territory. Journal of Clinical Neuroscience, 18 (2), 203-208.
Piven, J., Arndt, S., Bailey, J., & Andreasen, N. (1996). Regional brain enlargement in autism: a magnetic resonance imaging study. Journal of the American Academy of Child & Adolescent Psychiatry, 35 (4), 530-536.
Samson, F., Mottron, L., Soulières, I., & Zeffiro, T. A. (2012). Enhanced visual functioning in autism: An ALE meta‐analysis. Human Brain Mapping, 33 (7), 1553-1581.
Sperling, J. M., Prvulovic, D., Linden, D. E., Singer, W., & Stirn, A. (2006). Neuronal correlates of colour-graphemic synaesthesia: AfMRI study. Cortex, 42 (2), 295-303.
Tate, D. F., Bigler, E. D., McMahon, W., & Lainhart, J. (2007). The relative contributions of brain, cerebrospinal fluid-filled structures and non-neural tissue volumes to occipital-frontal head circumference in subjects with autism. Neuropediatrics, 38(01), 18-24.

